
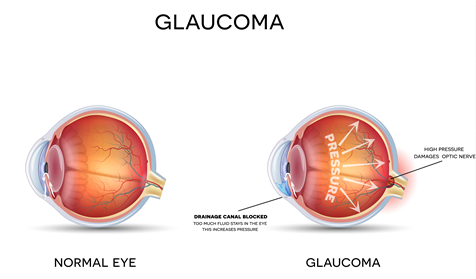
Glaucoma is a serious eye disease where progressive degeneration of the optic nerve results in gradual vision loss and it is usually the result of elevated eye (intraocular) pressure. Elevated eye pressure may occur due to a buildup of internal fluid (aqueous humor) that flows throughout the inside of the eye. This fluid normally drains out through the trabecular meshwork (the drainage channel of the eye). If the trabecular meshwork is not functioning properly or if there is an over-production of fluid, then an increase in eye pressure can occur.
EARLY DETECTION OF GLAUCOMA
Many people affected by glaucoma are not aware of any vision loss in the early stages of the disease. The loss of vision in glaucoma is usually gradual and peripheral (side) vision may be lost without prompt diagnosis and treatment. Once vision has been affected due to glaucoma, it cannot be recovered and “tunnel vision” at the end stage of glaucoma is commonly referred to. This is the reason why early detection is so important for protecting your sight. If glaucoma is detected and treated early, vision loss can be reduced or prevented.
WHAT ARE THE RISK FACTORS OF GLAUCOMA?
Age and family history are important risk factors of glaucoma. People over the age of 50 are at a greater risk of developing this eye disease and are encouraged to have eye examinations regularly. While glaucoma is more common as we get older, it is important to know that glaucoma can occur at any age. Anyone with a family history of glaucoma (especially in first-degree relatives) should have their eyes tested as there is a 10-fold risk of also developing the condition.
Risk factors of glaucoma include:
- Age
- Family history of glaucoma (especially first-degree relatives)
- Medical conditions such as diabetes, hypertension, and heart disease
- Being highly short-sighted or long-sighted
- History of eye injuries or eye surgeries in the past
- Taking medications such as corticosteroids including eyedrops
TYPES OF GLAUCOMA
Open-angle glaucoma
Open-angle glaucoma is the most common type of the disease. The drainage angle of the eye between the iris and the cornea is open but the trabecular meshwork may be partially blocked and not functioning properly. This results in an increase in eye pressure and progressive damage to the optic nerve.
Angle closure glaucoma
In angle closure glaucoma (also called closed-angle glaucoma), the drainage angle is closed, preventing the fluid to drain out of the eye resulting in an increase in eye pressure. The onset of angle closure glaucoma is usually sudden, and patients may experience symptoms such as severe headache, eye pain, blurred vision, eye redness, haloes around lights, vomiting and nausea. Acute angle-closure glaucoma is a medical emergency. If you experience any of the symptoms, you should be assessed and treated as soon as possible.
Normal tension glaucoma
Not all types of glaucoma are characterized by elevated eye pressures. In normal tension glaucoma, optic nerve may be progressively damaged even though the eye pressure is within a normal range. Causes may be due to limited blood supply or poor circulation and normal tension glaucoma needs to be appropriately managed.
HOW DO YOU TREAT GLAUCOMA?
Current glaucoma treatment works on the principles of enhancing the drainage of the fluid, reducing fluid production or bypassing the drainage system if it is obstructed. Depending on the type and stage of glaucoma, our doctors will advise the most appropriate treatment option following a comprehensive assessment. Investigations may include optic nerve analysis, corneal thickness and visual field testing.
Treatment options may include eyedrops, oral medications, laser treatment, eye surgery and minimally invasive glaucoma surgery (MIGS). MIGS involves small stent devices inserted in the eye to help drain the fluid to lower the pressure and/or reduce the need for glaucoma medications. Glaucoma surgery may involve making special drainage channels in the eye and sometimes using drainage tube devices in advanced cases.
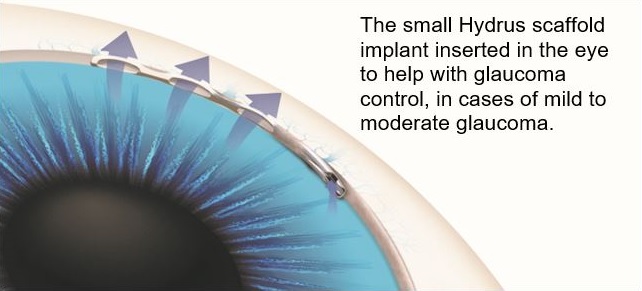
MIGS are now commonly performed in combination with your cataract surgery or as a standalone procedure. A common question from patients who have had stents is:
Can I have an MRI if I have had MIGS due to the small device implanted inside the eye?
Two common MIGS devices are iStent inject® and Hydrus Microstent®. The Hydrus Microstent® is a tiny scaffold inserted into the natural drainage channel of your eye to lower the eye pressure and/or reduce the need for medications. The device is made of nickel-titanium (nitinol) alloy and should not cause an allergic reaction. It is considered safe if you need to have an MRI scan and the device will not set off airport scanners.
The iStent inject® device is currently one of the smallest medical devices known to be implanted in the human body. Constructed from heparin-coated titanium, the iStent inject® is designed to optimize the outflow of fluid in the eye to reduce pressure. Patients who have had iStent inject® can also undergo MRI scans safely if meeting the following conditions: static magnetic field of 3T or less. Please speak to our doctors if you have any concerns.
There are now proven treatments that will effectively slow or halt the progression of glaucoma. City Eye Centre specialises in the diagnosis and management of glaucoma, including evidence-based medical, laser and surgical treatment options. We ensure the best management through the most current research and practice.
Call our team today to learn more about glaucoma and treatments. We are conveniently located on Wickham Terrace, Brisbane and at the Specialist Medical Centre in Sunnybank. Phone (07) 3831 6888 to book your appointment or email appointments@cityeye.com.au
