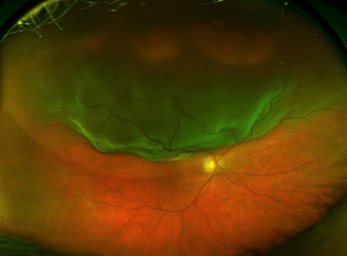
A retinal detachment is where the retinal lining detaches from the back wall of the eye. This is due to a tear or a break in the lining, allowing fluid from the vitreous jelly to leak under the retinal lining, causing the retina to lift off. The retinal tear may occur due to trauma, or more commonly, due to vitreous traction from the vitreous jelly causing a rip in the retinal lining.
Approximately one in ten thousand people will suffer from a retinal detachment. Prior eye surgery or trauma may increase the risk. In some cases, there may be a family history of retinal detachment. High myopia (short-sightedness) also increases the risk of retinal detachment. Some patients may be born with an inherited weakness in the retina causing lattice degeneration that may also pre-dispose them to a retinal detachment.
What are the symptoms of a retinal detachment?
Symptoms of a retinal tear or detachment include a sudden onset of flashes and floaters, followed by loss of vision, with the impression that there is a curtain moving up and down or sideways. They may note that vision on one side of their field has decreased. The patient may also notice that their vision is blurred. The retinal detachment may be associated with some haemorrhage into the vitreous jelly so some patients, in addition to the blurred vision, may notice a reddish or pinkish tinge to their vision.
Treatment of a retinal detachment
Treatment of a retinal detachment involves an operation. There are two methods that can be used to treat a retinal detachment.
1. Vitrectomy surgery
Vitrectomy surgery involves the removal of the vitreous jelly which can harbour factors that contribute to scarring and traction on the retina and subsequent detachment. Vitrectomy surgery uses advanced microscopic wide field viewing systems with microsurgical instruments inside the eye, enabling laser treatment to seal the retinal tear or break after the vitreous traction has been removed and the retina flattened with air, or heavy liquid. Diluted gas (C3F8 or SF6) is injected inside the eye to tamponade the retinal break. This is usually absorbed over a period of six to eight weeks where C3F8 is used. Alternatively depending on the configuration of the detachment and the need to travel by air, silicone oil, heavy silicone oil, or heavy liquid can be used as a tamponade agent though they will need to be removed at a later stage.
2. Scleral buckling
Scleral buckling surgery is rarely used and reserved for smaller retinal detachments, dialysis type of detachments or augmentation of the vitrectomy surgery.
A scleral buckling operation uses a reinforcing silicone band which is placed on the outer wall of the eye to close the retinal tear. This is used in conjunction with cryotherapy which seals the retinal tear or break. Air or gas may be injected into the eye which also helps to close the tear or break. The scleral buckle remains in place permanently and becomes part of the eye wall. In very rare circumstances, it may need to be removed at a future time.
The length of time for surgery varies from approximately 45minutes for a vitrectomy or scleral buckling operation to one and a half hours for a complicated case involving vitrectomy surgery and scleral buckling.
Anaesthesia
In most cases, vitrectomy surgery and scleral buckling can be performed under local anaesthetic with sedation. If required, general anaesthesia can be provided.
Success rate
The success rate for retinal detachment surgery is approximately 90%. Approximately 10% of cases may require further surgery if the retina is not attached after the first procedure. In some cases, the retina may be attached initially, but the retina may scar after about 6 to 10 weeks and re-detach requiring revision vitrectomy surgery. Once your retina remains attached for 3 months following the surgery, the incidence of further retinal detachment is much less.
Cataract surgery may be required in combination with the vitrectomy repair, or a later time once the retina is repaired.
Following a retinal detachment procedure, normal vision may not be fully regained. This is due to damage to the photoreceptor cells at the macula. The vision following retinal detachment surgery may continue to improve for up to a year following the surgery. The improvement in vision will depend on the amount of retinal detachment, if the macula was involved and the duration of a retinal detachment prior to the surgery.
