Diabetic retinopathy is a condition caused by diabetes mellitus where blood vessels of the retina are damaged due to high blood glucose level. Such damage to the blood vessels of the retina can result in abnormal bleeding (retinal haemorrhages) and swelling of the retina (macular oedema). It can also cause poor blood flow to the retina (ischaemia) and/or scarring of the retina. It can occur for both Type I and Type II diabetes. The longer you have had diabetes, the more likely you are to develop diabetic retinopathy. Moreover, the less well-controlled the diabetes, the more likely it is also to develop diabetic retinopathy.

What are the Types of Diabetic Retinopathy?
There are two types: non-proliferative diabetic retinopathy (NPDR) and a more severe form, proliferative diabetic retinopathy (PDR). In NPDR, the damaged retinal blood vessels develop tiny weak areas called microaneurysms. Over time, these microaneurysms can rupture and leak, resulting in retinal haemorrhages (bleeding). Fluid, fats, and protein from the bloodstream can leak into the retina and cause swelling (oedema) and hard exudates. Poor blood circulation of the retina can also result in the death of nerve cells (ischaemia). The combination of these processes can lead to permanent vision loss.
In proliferative diabetic retinopathy (PDR), the retina can produce substances that promote the growth of new, abnormal blood vessels (neovascularization) in response to the ischaemia. These new blood vessels are fragile and tend to bleed into the vitreous. This can result in scar tissues that pull on the retina. Potentially, it can cause a very serious condition called tractional retinal detachment.
What Tests are Required?
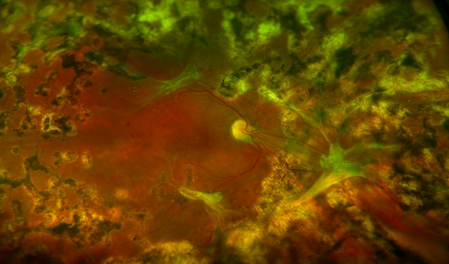
When diabetic retinopathy is diagnosed, you may need to undergo further investigations. These include fluorescein angiography, OCT scan, and OCT angiography. The purpose of these investigations is to evaluate the severity of the condition and identify areas of macular oedema, ischaemia and neovascularisation. This ensures appropriate treatments can be applied. Furthermore, a B-scan ultrasound may need to be performed when the vitreous haemorrhage is very dense. This is necessary if the retina cannot be examined properly.
Diabetic Control
The most important aspect in the treatment of diabetic retinopathy is adequate long-term control of blood glucose levels. Patients should monitor their glucose and have their haemoglobin A1c level checked with their GP. Regular eye examinations are important. Symptoms of blurred vision or floaters only appear long after diabetic retinopathy has developed. Therefore, early detection and treatment before the retina is severely damaged is the most successful in minimizing visual loss from diabetic retinopathy. In addition, it is a good idea to keep blood pressure and cholesterol levels in check.
What Types of Treatment are There?
Intravitreal therapy such as Eylea, Eylea HD and Ozurdex may be necessary to treat macular oedema as well as new vessels in diabetic retinopathy. These drugs are highly effective, though regular review and treatment are required. Also, treatment may need to be repeated at regular intervals to continue long-term benefits. In some cases, these drugs are combined with vitrectomy surgery.
PANRETINAL PHOTOCOAGULATION (PRP)
Panretinal photocoagulation laser surgery is performed in proliferative diabetic retinopathy patients to prevent severe vitreous haemorrhages and blindness. The laser causes regression of abnormal blood vessels. Each laser session takes approximately fifteen to twenty minutes. Usually, multiple sessions are required. There may be some discomfort during the laser treatment. Analgesics such as Panadol or Nurofen may be taken before the treatment. With time, one may notice some decrease in night vision and peripheral vision due to the laser treatment. This is, however, necessary to control the proliferative diabetic retinopathy.
In severe cases of proliferative diabetic retinopathy where laser surgery is unsuccessful, vitreoretinal surgery might be indicated. Vitreoretinal surgery involves the use of microsurgical instruments inside the eye to remove scar tissue and haemorrhage in the vitreous jelly. Laser treatment can also be performed during surgery. In addition, a special gas bubble is placed inside the eye which absorbs naturally over a few weeks. Vision may improve following surgery over several months. The improvement depends on the state of the eye prior to the surgery. Risks with diabetic vitrectomy include further haemorrhages into the eye, retinal detachment and cataract formation. Any of these complications may necessitate further surgery.
